Prostate Enlargement (BPH)
- Home
- Treatments
- Prostate Enlargement (BPH)
Benign Prostatic Hyperplasia (BPH)
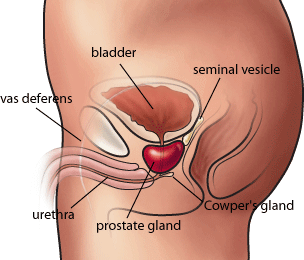
What You Should Know About Your Prostate
HOW DOES BPH PRESENT?
- P – Poor flow (Weak stream)
- I – Intermittency (interrupted urine flow)
- S – Strain to pass urine
- S – Sense of incomplete voiding (incomplete emptying)
- F – Frequency (Increased frequency of urination)
- U – Urgency (Inability to hold urine)
- N – Nocturia (Increased frequency at night)
Circle your answer and write your score in the right-hand column. Talk with your provider if your total score is 8 or greater or if you are bothered at all.
| Not at all | Less than 1 time in 5 | Less than half the time | About half the time | More than half the time | Almost always | Your score | |
| Incomplete emptying? It does not feel like 1 empty my bladderall the way. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Frequency? 1 have to go again less than two hours after 1 finishurinating. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Intermittency? 1 stop and start again several times when 1urinate. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Urgency? It is hard to wait when 1 nave to urinate. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Weak stream? 1 have a weak urine stream. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Straining? 1 have to push or strain to begin urination. | 0 | 1 | 2 | 3 | 4 | 5 | |
| None | 1 time | 2 times | 3 times | 4 times | 5 times or more | Your score | |
| Nocturia? 1 get up to urinate after 1 go to bed until the time 1get up in the morning. | 0 | 1 | 2 | 3 | 4 | 5 | |
| Total AUA Symptom Score | |||||||
| Total score:0-7 mildly symptomatic; 8-19 moderately symptomatic; 20-35 severely symptomatic | |||||||
| Quality of life due to urinary symptoms | Delighted | Pleased | Mostly satisfied | Mixed: about equally satisfied and dissatisfied | Mostly dissatisfied | Unhappy | Terrible |
| If you were to spend the rest of your life with your urinarycondition just the way it is now,how would you feel about that? | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
Throughout their lives, men produce testosterone, a male hormone, and small amounts of estrogen, a female hormone. As men age, the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen. Scientific studies have suggested that benign prostatic hyperplasia may occur because the higher proportion of estrogen within the prostate increases the activity of substances that promote prostate cell growth.
Another theory focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT in the prostate. This accumulation of DHT may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce DHT do not develop benign prostatic hyperplasia.
- Urinalysis (urine test)
- PSA blood test to screen for prostate cancer
- Urinary blood test to screen for bladder cancer
- Post-void residual volume (PVR) to measure urine left in the bladder after urinating
- Ultrasound of the prostate
- Uroflowmetry to measure how fast urine flows
- Urodynamic pressure to test pressure in the bladder during urinating
- Cystoscopy to look at the urethra or bladder with a scope is needed in special situations ONLY
PSA Test
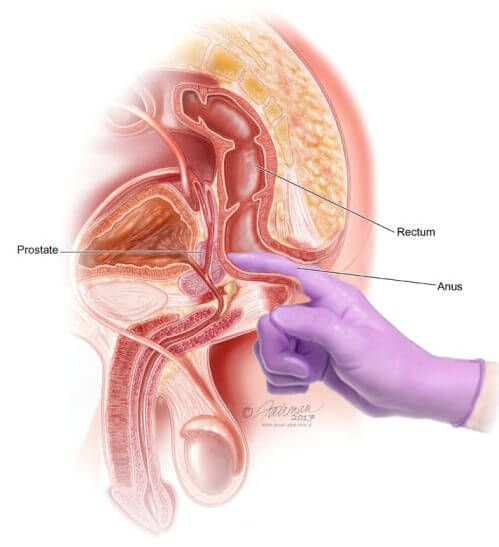
DRE
How is BPH Treated?
The main treatments for BPH are:
Watchful waiting
BPH is monitored but there is no active treatment. Diet and medicine can control symptoms. You will have a yearly exam. Your doctor will look for worse or new symptoms before beginning active treatment.
What Are the Benefits, Risks and Side Effects of Watchful Waiting/Active Surveillance?
There are no side effects.
Who Are Good Candidates for Watchful Waiting/Active Surveillance?
Men with mild symptoms may be good candidates for this treatment. Men with moderate symptoms who are not bothered by the symptoms are also good candidates.
What do you do?
Few life-style changes are very important
- Avoid excessive liquids
- Avoid diuretics (Things that produce excess urine like excess tea, coffee, soft drinks, beer)
- Do not try to hold urine
- Avoid constipation
- Reduce liquids two hours before bed-time.
Medical therapies
Many groups of drugs are available that will alleviate your urinary symptoms. The choice of drugs is dependent on the amount of your symptoms, the size of your prostate and the status of your sexual life. It is very important to discuss with your doctor about expectations in your sexual life. The drugs could be chosen based on what you expect. The life-style changes described above also apply when drug therapy is given.
Alpha Blockers
What are The Benefits, Risks and Side Effects of Alpha Blockers?
Who Are Good Candidates for Alpha Blockers?
What Are 5-Alpha Reducatase Inhibitors?
5-Alpha reducatase inhibitors block the production of dihydrotestosterone (DHT). DHT is a male hormone that plays a role in prostate development and growth. DHT accumulates in the prostate and may cause prostate growth. 5-Alpha reducatase inhibitors are pills that increase urine flow and shrink the prostate. These drugs include finasteride and dutasteride.
What Are The benefits, Risks and Side Effects of 5-Alpha Reducatase Inhibitors? These drugs lower the risk of BPH complications. They lower the need for surgery. Side effects are sexual, such as erectile dysfunction and reduced libido (sex drive). You must take them indefinitely to prevent symptoms.
Who Are Good Candidates for 5-Alpha Reducatase Inhibitors?
These drugs may be best for men with very large prostate glands. Older men are good candidates. PDE5 inhibitors
Low dose PDE5 inhibitors have good effect on the urinary symptoms. The added benefit would be it would also improve your sexual life. This is a preferred drug for men who are keen on maintaining or improving their sexual life.
What is Combination Therapy?
Combination therapy uses an alpha blocker and a 5-alpha reducatase inhibitor together. Several studies, such as the Medical Therapy of Prostatic Symptoms (MTOPS) study, have shown that combining two classes of medications, instead of using just one, can more effectively improve symptoms, urinary flow, and quality of life.
A urologist may prescribe a combination of alpha blockers and antimuscarinics for patients with overactive bladder symptoms. Overactive bladder is a condition in which the bladder muscles contract uncontrollably and cause urinary frequency, urinary urgency, and urinary incontinence. Antimuscarinics are a class of medications that relax the bladder muscles.
What Are the Benefits, Risks and Side Effects of Combination Therapy?
Alpha blockers and 5-alpha reducatase inhibiters work better together than either one alone. They prevent BPH from getting worse. They improve symptoms. But there may be more side effects. There may be side effects from each drug.
Who Are good candidates for combination therapy?
Men with larger prostates are good candidates for this treatment.
What Are Phytotherapies?
These are herbal therapies. They are very popular. They are “self treatment.” They are not prescribed by a health care provider. One popular herb is saw palmetto.
What Are the Benefits, Risks and Side Effects of Phytotherapies?
Herbal treatments have not been proven to work. In fact, some studies show they do not work. Also, the quality and purity of these over-the-counter supplements vary
Who are Good Candidates for Phytotherapies?
This treatment is not currently recommended by health care providers.
Minimally Invasive Surgeries
Minimally invasive surgeries can be done in your doctor’s office or an outpatient center. Choosing the right surgery for you may depend on:
- The size of your prostate.
- How healthy you are.
- Your personal choice.
There are several types of minimally invasive procedures to choose from, they include: Prostatic Stent
- Transurethral Microwave Thermotherapy (TUMT)
- Transurethral Needle Ablation (TUNA)
- Photoselective Vaporization (PVP)
- UroLift
- Catheterization
What Are the Benefits, Risks, and Side Effects of Minimally Invasive Surgeries?
Getting relief from your symptoms is the biggest benefit of having minimally invasive surgery. In addition, some men have fewer problems controlling their urine after they have one of these types of surgeries. However, by having a minimally invasive surgery, you may be at a higher risk for needing another surgery in the future. Side effects from minimally invasive surgery may include:
- Erectile dysfunction issues.
- Semen flowing backward into the bladder instead of out of the penis (retrograde ejaculation).
- Urinary Tract Infection.
- Blood in your urine.
- Burning with urination.
- Needing to urinate more often.
- Sudden urges to urinate.
Who Are Good Candidates for Minimally Invasive Surgeries?
Men who are having trouble urinating are good candidates for a minimally invasive surgery. In addition, you may be a good candidate for this type of surgery if you:
- Have symptoms that are moderate to severe.
- Can’t empty your bladder completely.
- Urinate very slowly
- Have taken medications and they did not work
What is A Prostatic Stent?
The stent is a spring-like device. It is placed inside the urethra. The stent holds the urethra open. There are many kinds of stents.
Who Are Good Candidates for Prostatic Stents?
Men with many medical problems may be good candidates. Men for whom surgery is high-risk may also be good candidates.
Prostatic stents are used for men who would otherwise use a catheter or transurethral microwave thermotherapy (TUMT). You should not get the stent if your urethra is narrow. You should not get a stent if you have urinary infection, bladder stones, weak bladder or cancer. And you should not get a stent if you will soon have urethra treatments for kidney stones.
What is Photoselective Vaporization (PVP)?
Photoselective vaporization of the prostate (PVP) uses a high-powered laser. It is also called as ‘green-light laser.’ The laser vaporizes the obstructing prostate tissue.
What Are the Benefits, Risks and Side Effects of PVP?
PVP is becoming very popular. Most men can have a PVP without adverse events. PVP is replacing more invasive surgery. It is done in the office or as an outpatient at the hospital. There is little bleeding. There are few side effects. After PVP, you can often stop medical therapy.
Who Are Good Candidates for PVP?
Good candidates include men with too many medical problems for invasive surgery. Men with weak hearts are good candidates because there is no blood loss. So are men who want to limit anesthesia.
What is UroLift?
UroLift opens the blocked urethra. It lifts and holds the enlarged prostate out of the way. Small implants are delivered through a needle. The goal is to relieve symptoms. Sadly as of 2018, this treatment is yet not available in India.
What Are the Benefits, Risks and Side Effects of UroLift?
With UroLift, health care providers do not have to cut into your body, destroy the prostate or remove any tissue. With UroLift men may have fewer sexual side effects than with other minimally invasive surgeries.
Who Are Good Candidates for UroLift?
Most men with enlarged prostates and urinary symptoms may be good candidates for this treatment. In some men, symptoms that remain after treatment are from another source. Men who have this treatment can still have other treatment if they need it.
What Is Catheterization?
This treatment places a tube called a catheter into the bladder. The tube drains urine. Catheters are of three types:
- Clean intermittent catheter: Placed and removed every six to eight hours. Clean catheterization can be done by you or a caregiver. Clean catheterization is when you remove the catheter once the flow of urine has stopped; no tubes are left in the bladder.
- Indwelling: Left in the bladder for short or long period of times.
- SuprapubicCatheters: Placed into the bladder through a small puncture in the bladder above the pubic bone.
What are the benefits, risks and Side Effects of Catheterization?
Catheters’ benefits are temporary. Infection is the biggest risk of having a catheter in place for long periods. Bacteria can stick to the surface of the catheter. This makes it hard for the immune system or antibiotics to work. After a few years, there is a higher risk of bladder cancer. This is probably due to the long-term irritation from the catheter sitting in the bladder. Clean intermittent catheterization (CIC) has lower risk of infection and cancer than an indwelling catheter.
Who are good candidates for Catheterization?
Good candidates for a catheter include men waiting for medication to work or for surgery who are unable to pass urine. Catheters are also used during treatment for an infection. They may be a good choice for men with multiple medical problems and a short life expectancy. The risk and discomfort of surgery may outweigh the risk of infection or cancer. Catheterization is chosen over medications or surgery for men with bladder control problems and a blocked prostate.
Surgical intervention
When medical therapy fails and in severe cases, surgery can remove obstructing prostate tissue. Surgery is almost always recommended if you:
- Are unable to urinate
- Have kidney damage
- Have frequent urinary tract infections
- Have a lot of bleeding
- Have stones in the bladder
What is Transurethral Resection of the Prostate (TURP)?
Transurethral Resection of the Prostate (TURP) is the most common surgery for BPH. TURP uses electric current to resect prostate in small chips.
After anesthesia, the surgeon inserts a resectoscope through the tip of the penis into the urethra. The resectoscope has a light, valves for irrigating fluid, and an electrical loop. The loop cuts tissue and seals blood vessels. The removed tissue flushes into the bladder and out of the body. A catheter is placed in the bladder through the penis.
What are the benefits, risks and side effects of TURP?
This treatment has excellent outcomes. All treatments are generally compared with it. There are no cuts. The hospital stay is 3 to 4 days. The catheter may be removed before you go home. Or it may be removed later as an outpatient. This surgery does require anesthesia. As with any surgery, anesthesia poses a risk.
Who are good candidates for TURP?
Men who require surgery may be good candidates for TURP. It does not remove the entire prostate. There may be less need for further treatment with TURP.
What is Transurethral Incision of the Prostate (TUIP)?
Transurethral incision of the prostate (TUIP) is used if you have a smaller prostate gland but major blockage. Instead of cutting and removing tissue, this procedure widens the urethra. The surgeon makes small cuts in the bladder neck, where the urethra joins the bladder, and in the prostate. This reduces the pressure of the prostate on the urethra. It makes urination easier. The hospital stay is one to three days. A catheter is left in your bladder for one to three days after surgery.
What are the benefits, risks and side effects of TUIP?
TUIP may improve the ability to urinate. It may ease symptoms. Temporary urine retention, urinary tract infection, dry orgasm (climax), incontinence and erectile dysfunction may happen. Some men need follow-up treatment.
Who are good candidates for TUIP?
Men who do not want a complete prostatectomy (removal of the prostate) but need surgery are good candidates for TUIP.
What is Holmium Laser Enucleation of Prostate (HoLEP)?
With holmium laser enucleation of prostate (HoLEP), the surgeon places a resectoscope through the penis into the urethra. The laser completely enucleates the obstructing prostatic adenoma. The tissue is then morcellated in the bladder and removed as a mince-meat
What are the benefits, risks and side effects of HoLEP?
There is very little bleeding. There is a short recovery time. You will need a catheter, but it is usually removed the next day. You will only stay 1-2 night in the hospital. But, this treatment requires anesthesia. As with any surgery, anesthesia poses a risk.
It has a major advantage in patients with very large prostates. Prostates as big as 200-250 Grams can be comfortably removed by HoLEP. In contrast TURP is not advisable for glands more than 80-100 Grams. HoLEP can be performed in patients who are on anti-platelet agents.
It has a higher chance of maintaining sexual function post-treatment.
Who are good candidates for HoLEP?
Men with larger prostates who wish to avoid more invasive surgery may be good candidates for this treatment.
After Treatment
What Happens After Treatment?
For most men, symptoms improve after treatment. Infection, bleeding, incontinence, and erectile dysfunction may occur after some treatments. In some cases, scar tissue may form. There may be complications after surgery. Some men need further or new treatment.
What are the long term side effects of treatment?
Side effects vary with the type of treatment you choose. Most side effects are temporary. It may take a while for sexual function to return fully. Most experts agree that if you were able to have an erection shortly before surgery, you will probably be able to after surgery. Most men find little or no difference in orgasm. They may have retrograde ejaculation. This is when semen enters the bladder rather than being sent out. For most men, side effects lessen with time. But there may be long term side effects for some men for some treatments.
The long term complications may include stricture in urethra (narrowing of the urinary outlet tube), Bladder neck contracture (narrowing at the site where the prostate and bladder join) or re-growth of prostate. Stricture and contracture may form within first two years of the treatment. Regrowth may take 8-10 years.
How can you prevent a recurrence of BPH?
Once you have been treated, taking medication continually can prevent BPH symptoms from returning or getting worse. In some men, a different treatment may be necessary. Some men they will need repeated treatments to get rid of bothersome symptoms. In older men, it may be possible to control the symptoms of BPH to the end of life.
